Preventive health care expenditure statistics
Data extracted in March 2023.
Planned article update: 23 May 2024.
Highlights
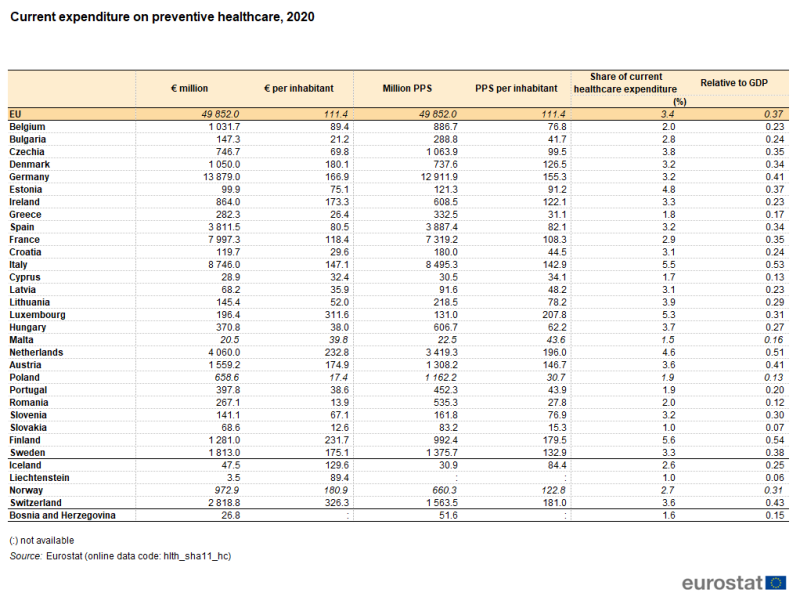
EU Member States spent €49.9 billion on preventive health care in 2020; note that this was the first year of the COVID-19 crisis.
Preventive health care expenditure in the EU was equivalent to 0.37 % of GDP in 2020.
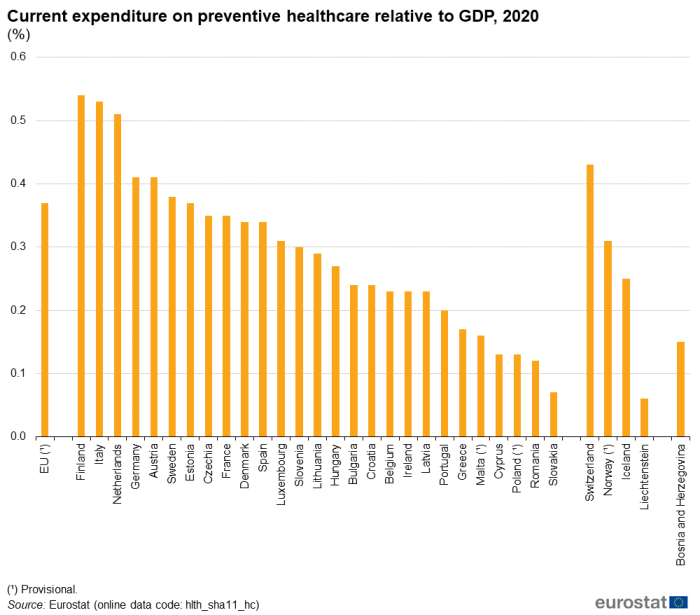
Current expenditure on preventive healthcare relative to GDP, 2020
This article forms part of the online publication Health in the European Union and more specifically is part of the domain of healthcare expenditure statistics. It presents key statistics on preventive healthcare expenditure in the European Union (EU) for the reference year 2020. With the release of 2020 data, the data in this article relate information on preventive healthcare expenditure during the first calendar year of the COVID-19 crisis.
Within the health sector, preventive care involves 'any measure that aims to avoid or reduce the number or severity of injuries and diseases, their sequelae and complications' [1]. It is based on a health promotion strategy that enables people to improve their health by controlling some immediate determinants [2]. Preventive healthcare includes interventions for both individual and collective consumption.
According to the 2011 edition of the system of health accounts (SHA 2011), preventive healthcare aims to reduce the 'risks before they generate some effects' [3] and to detect diseases as early as possible. Activities aimed at 'reducing the negative impact of an already established disease or injury by an attempt to avoid worsening and complications and then therapy' are therefore outside the scope of preventive healthcare [4]. For some countries, it can be difficult to identify expenditure on preventive healthcare separately from expenditure on curative and rehabilitative care [5], leading to an underestimation in this area.
Full article
Preventive healthcare in the EU accounted for 0.37 % of GDP in 2020
Finland, Italy and the Netherlands spent the highest amount on preventive healthcare relative to GDP in 2020
Expressed in euros, expenditure on preventive healthcare provides a measure of a country's financing of this function of health care. To some extent, the level reflects the size of the economy. By analysing current expenditure on preventive healthcare in absolute terms (euros) and also relative to GDP, a comprehensive overview of different levels of expenditure can be seen. To put spending in absolute terms into perspective, based on the size of the population in each EU Member State (see population change – demographic balance and crude rates at national level), a specific section on expenditure per inhabitant is provided later in this article.
With 0.54 %, 0.53 % and 0.51 % of their gross domestic product (GDP), Finland, Italy and the Netherlands had the highest expenditure ratios for preventive healthcare in 2020 among the EU Member States. Germany and Austria (both 0.41 %) were the only other Member States where expenditure on preventive healthcare was more than 0.40 % of GDP in the same reference year (see Table 1 and Figure 1).
Slovakia (0.07 %) recorded the lowest ratio and was the only EU Member State to allocate less than 0.10 % of its GDP to expenditure on preventive healthcare in 2020.
(%)
Source: Eurostat (hlth_sha11_hc)
In absolute terms, total expenditure on preventive healthcare for all EU Member States amounted to €49.9 billion in 2020.
- Germany spent €13.9 billion on preventive healthcare, recording the highest value among Member States; it was also the only Member State to spend more than €10 billion.
- Four other Member States spent more than €3.0 billion on preventive healthcare in 2020: Italy (€8.7 billion), France (€8.0 billion), the Netherlands (€4.1 billion) and Spain (€3.8 billion).
- At the other end of the ranking, Cyprus (€28.9 million) and Malta (€20.5 million) recorded the lowest values across the EU.
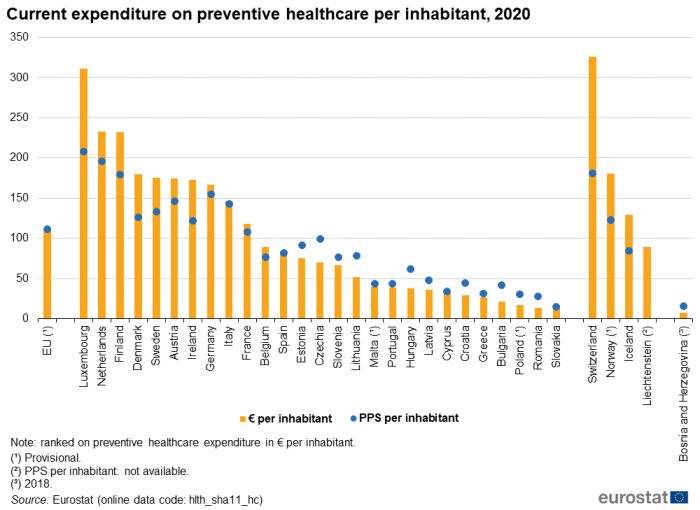
Ten EU Member States spent more than €100 per inhabitant on preventive healthcare in 2020
With expenditure of €311.6 per inhabitant, Luxembourg spent the most relative to its population size
Taking into account the size of the population, Luxembourg led the ranking among EU Member States, having spent €311.6 per inhabitant on preventive healthcare in 2020. Two other EU Member States recorded expenditure above €200.0 per inhabitant: the Netherlands (€232.8) and Finland (€231.7). At the other end of the scale, Romania (€13.9) and Slovakia (€12.6) reported the lowest values per inhabitant in 2020. The ratio between the highest and lowest levels of preventive healthcare expenditure per inhabitant – based on a comparison between Luxembourg and Slovakia – was therefore 24.8 : 1.
Among the European Free Trade Association (EFTA) countries, Switzerland recorded the highest per inhabitant expenditure on preventive healthcare (€326.3) in 2020, which was also higher than in any of the EU Member States.
Table 1 shows the level of expenditure on preventive healthcare measured in purchasing power standards (PPS), an artificial currency unit that takes account of the price level differences between EU Member States; these data expressed in relation to the number of inhabitants are also shown in Figure 2.
- Germany had the highest value in absolute terms in 2020, with expenditure on preventive healthcare of 12.9 billion PPS.
- Based on the ratio of preventive healthcare expenditure per inhabitant (measured in PPS terms), Luxembourg (207.8 PPS per inhabitant) spent the most on preventive healthcare, followed by the Netherlands, Finland and Germany, all with values above 175.0 PPS per inhabitant.
- Slovakia was at the other end of the ranking, with expenditure of 15.3 PPS per inhabitant in 2020.
From Figure 2, it can clearly be seen that EU Member States with relatively high levels of expenditure on preventive healthcare per inhabitant in euro terms tended to have lower ratios in PPS terms; the reverse was observed for Member States with relatively low levels of expenditure. Unsurprisingly therefore, the ratio between the highest and lowest levels of preventive healthcare expenditure per inhabitant when measured in PPS (taking account of price level differences) – based on a comparison between Luxembourg and Slovakia – was considerably less (13.6 : 1) in 2020 than the ratio in euro terms (24.8 : 1).
Source: Eurostat (hlth_sha11_hc)
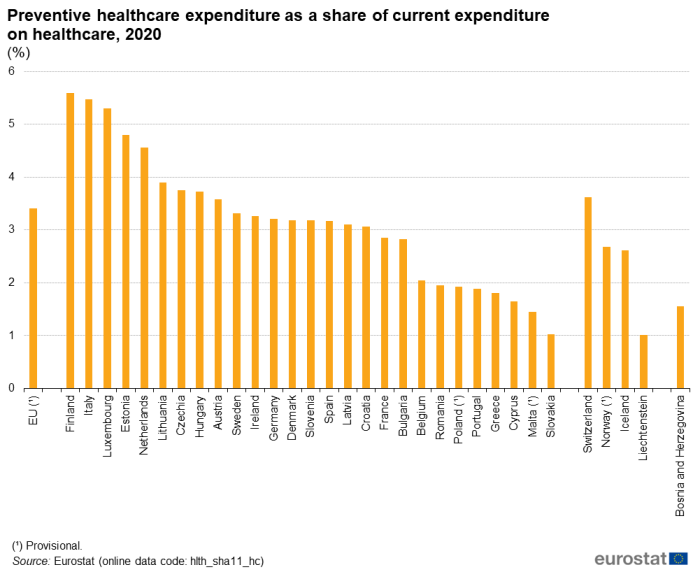
Among EU Member States, spending on preventive healthcare ranged between 1.0 % and 5.6 % of current healthcare expenditure in 2020
Finland, Italy and Luxembourg spent the highest share of health expenditure on preventive healthcare
Ranging from a peak of 5.6 % of current healthcare expenditure to a low of 1.0 %, preventive healthcare is a relatively small function within the system of health accounts (see Figure 3).
In 2020, the share of preventive healthcare expenditure in total health expenditure was highest in Finland at 5.6 %, closely followed by Italy (5.5 %) and Luxembourg (5.3 %). In six other EU Member States, this share was also above the EU average (3.4 %). At the other end of the ranking, six Member States reported shares below 2.0 %: Poland, Portugal (both 1.9 %), Greece (1.8 %), Cyprus (1.7 %), Malta, (1.5 %) and Slovakia (1.0 %).
(%)
Source: Eurostat (hlth_sha11_hc)
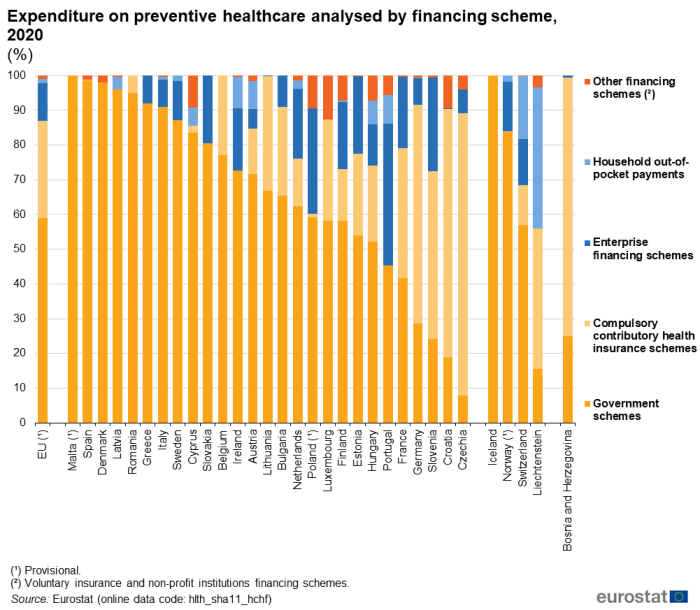
Preventive healthcare mainly financed by government schemes
In Malta, Spain and Denmark, preventive healthcare was almost entirely financed by government schemes in 2020
Healthcare financing schemes are a structural component of healthcare financing systems: they are the types of financing arrangements through which people obtain health services [6].
As indicated in Figure 4, government schemes were the main mechanism for financing preventive healthcare in 2020 in 23 of the EU Member States. Shares varied among these 23 Member States from 41.7 % in France and 45.2 % in Portugal to more than 50.0 % in the others, peaking at 98.0 % in Denmark, 98.7 % in Spain and 100.0 % in Malta. On average, government schemes financed 58.9 % of preventive healthcare across the EU in 2020.
Compulsory contributory health insurance schemes and compulsory medical saving accounts (CMSA) (which are generally part of the social security system) were the second largest financing mechanism with a share of 28.0 % of total preventive healthcare expenditure in the EU in 2020. They were the main financing scheme in the remaining four EU Member States: Czechia (81.5 %), Croatia (71.5 %), Germany (63.1 %) and Slovenia (48.2 %).
Enterprise financing schemes accounted for 11.0 % of preventive healthcare expenditure in the EU in 2020. In 11 EU Member States this share exceeded 10.0 %, peaking at 40.9 % in Portugal. With an average share of 1.1 %, household out-of-pocket payments did not play a significant role in the financing of preventive healthcare in the EU in 2020. The relative contribution of this means of financing exceeded 5.0 % in Cyprus, Hungary, Austria and Portugal as well as in Ireland where the share peaked at 9.1 %.
(%)
Source: Eurostat (hlth_sha11_hchf)
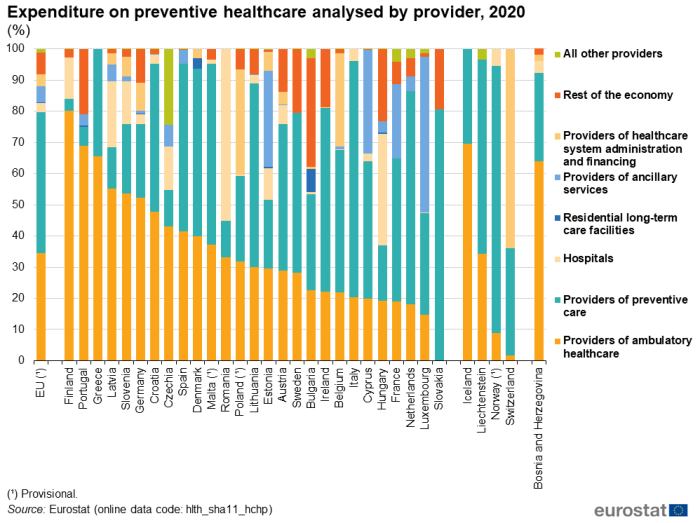
Preventive healthcare mainly delivered by providers of preventive health care in 2020
Providers of preventive care were the main providers of preventive healthcare in 13 EU Member States in 2020
Healthcare providers are 'organisations and actors that deliver healthcare goods and services as their primary activity, as well as those for which healthcare provision is only one among a number of activities. They vary in their legal, accounting, organisational and operating structures' [7].
As shown in Figure 5, there were two main providers of preventive healthcare.
- Providers of preventive care, which include 'organisations that primarily provide collective preventive programmes and campaigns/public health programmes for specific groups of individuals or the population as a whole, such as health promotion and protection agencies or public health institutes as well as specialised establishments providing primary preventive care as their principal activity' [8].
- Providers of ambulatory healthcare, defined in the system of health accounts as 'establishments that are primarily engaged in providing healthcare services directly to outpatients who do not require inpatient services. This includes both offices of general medical practitioners and medical specialists and establishments specialising in the treatment of day-cases and in the delivery of home care services' [9].
In 2020, there were nine EU Member States where providers of preventive care accounted for an absolute majority of current expenditure on preventive healthcare and in four more these providers accounted for just under half of all expenditure but for more than any other type of provider. The largest shares of expenditure for providers of preventive care were observed in Slovakia (80.6 %), Italy (75.7 %) and the Netherlands (68.3 %). In the EU, the share for providers of preventive care was 45.2 %.
Providers of ambulatory healthcare accounted for an absolute majority of current expenditure on preventive healthcare in six of the EU Member States and in two more these providers accounted for just under half of the total but for more than any other type of provider. The largest share of expenditure recorded for providers of ambulatory healthcare was observed in Finland (80.2 %). In the EU, the share for providers of ambulatory healthcare was 34.4 %.
In six EU Member States, the largest provider of preventive healthcare in 2020 was not one of these two types of providers – preventative care or ambulatory healthcare – which dominated for the EU as a whole.
- The rest of the economy accounted for 34.7 % of preventive healthcare expenditure in Bulgaria. This heading encompasses households as providers of home health care and other industries as secondary providers of health care. For comparison, the average share in the EU was 6.9 %.
- In Luxembourg and Estonia, providers of ancillary services had the largest share of preventive healthcare expenditure, 50.0 % and 30.7 %, respectively. The EU average was 5.2 %.
- Providers of healthcare system administration and financing accounted for 33.5 % of preventive healthcare expenditure in Poland. The average share in the EU was 3.8 %.
- In Romania and Hungary, hospitals had the largest share of preventive healthcare expenditure, 55.2 % and 35.7 %, respectively. The EU average was 3.0 %.
(%)
Source: Eurostat (hlth_sha11_hchp)
Source data for tables and graphs
![]() Preventive healthcare expenditure data: tables and figures
Preventive healthcare expenditure data: tables and figures
Data sources
Tables in this article use the following notation:
- values in italic show where a value is provisional;
- a colon ‘ : ‘ is used to show where data are not available.
Key concepts
Current expenditure on health care equals 'final consumption expenditure of resident units on health care goods and services, including the health care goods and services provided directly to individual persons as well as collective health care services' [10].
Healthcare expenditure is primarily concerned with healthcare goods and services that are consumed by resident units, irrespective of where that consumption takes place (it may be in the rest of the world) or who is paying for it. As such, exports of healthcare goods and services (to non-resident units) are excluded, whereas imports of healthcare goods and services for final use are included.
System of health accounts
Eurostat, the Organisation for Economic Co-operation and Development (OECD) and the World Health Organisation (WHO) established a common framework for a joint healthcare data collection exercise. The data collected relate to healthcare expenditure following the system of health accounts (SHA) methodology.
The system of health accounts shares the goals of the system of national accounts (SNA) 'to constitute an integrated system of comprehensive, internally consistent and internationally comparable accounts, which should as far as possible be compatible with other aggregated economic and social statistical systems'. Health accounts provide a description of the financial flows related to the consumption of healthcare goods and services from an expenditure perspective. Health accounts are used in two ways:
- internationally, where the emphasis is on a selection of comparable expenditure data;
- nationally, with more detailed analyses of healthcare spending and a greater emphasis on comparisons over time.
In 2011, and as a result of four years of extensive and wide-reaching consultation, Eurostat, the OECD and the WHO released an updated manual for the collection of health accounts, A System of Health Accounts 2011, revised edition. The core set of SHA tables addresses three basic questions.
- What kinds of healthcare goods and services are consumed?
- Which healthcare providers deliver them?
- Which financing schemes are used to deliver them?
Healthcare expenditure is recorded based on the international classification for health accounts (ICHA).
- Healthcare expenditure by financing schemes (ICHA-HF) – which classifies the types of financing arrangements through which people obtain health services; healthcare financing schemes include direct payments by households for services and goods and third-party financing arrangements.
- Healthcare expenditure by function (ICHA-HC) – which details the split in healthcare expenditure following the purpose of healthcare activities, such as, curative care, rehabilitative care, long-term care or preventive care.
- Healthcare expenditure by provider (ICHA-HP) – which classifies units contributing to the provision of healthcare goods and services, such as hospitals, residential facilities, ambulatory healthcare services, ancillary services or retailers of medical goods.
OECD guidelines for reporting preventive care have been published as Expenditure on Prevention Activities under SHA 2011: Supplementary Guidance - March 2017 version.
Healthcare expenditure – methodology
Commission Regulation (EU) 2015/359 of 4 March 2015 as regards statistics on healthcare expenditure and financing established the collection of data on healthcare expenditure according to SHA 2011 methodology. This Regulation applied to data from reference years 2014 until 2020. Commission Regulation (EU) 2021/1901 of 29 October 2021 as regards statistics on healthcare expenditure and financing will cover data from the 2021 reference year. These Regulations lay down rules for the development and production of European statistics in the area of healthcare expenditure and financing.
The information for the most recent years shown in this article therefore presents a harmonised set of data based on this methodology.
The background article Healthcare expenditure statistics – methodology documents healthcare expenditure statistics. It provides more information on the scope of the data, the legal framework, the methodology employed, as well as related concepts and definitions.
Context
Health systems across the globe are developing in response to a multitude of factors, including:
- new medical technology and improvements in knowledge;
- new health services and greater access to them;
- changes in health policies to address specific diseases and demographic developments;
- new organisational structures and more complex financing mechanisms.
However, access to healthcare and greater patient choice is increasingly being considered against a background of financial sustainability.
Europe is home to some of the lowest levels of income/wealth inequality, as well as some of the highest standards for working conditions and broad social protection. In 2017 at the Gothenburg Summit, the European Parliament, the Council and the European Commission proclaimed the European Pillar of Social Rights. This set out 20 key principles for guiding the EU towards a strong, social Europe that is fair, inclusive and full of opportunity in the 21st century. Under the action plan for social protection and inclusion, the European Commission acts to promote health and care systems; these have been under considerable strain during the COVID-19 pandemic. Reforms and investments in health systems are required to:
- increase their resilience and capacity to manage current and future crises;
- reinforce primary health care and mental health;
- improve access to quality health care for all and reduce social, territorial and economic inequalities in health.
The European Commission aims to build a strong European Health Union in which all EU Member States prepare and respond together to health crises, where medical supplies are available, affordable and innovative, and where countries work together to improve prevention, treatment and aftercare for diseases.
The European Commission has adopted strategic plans for the period 2020–2024 to translate President von der Leyen's six headline ambitions. In order to improve the quality and effectiveness of public expenditure and contribute to prosperity and social cohesion, the European Commission seeks to provide expertise on health systems and support actions that help prevent and reduce the impact of ill-health on individuals and economies, while encouraging and supporting innovation and the uptake of modern technologies for better care delivery and cost-effectiveness [11].
The Directorate-General for Health and Food Safety has established a list of 88 European core health indicators (ECHIs) for monitoring progress across the EU in relation to health policy and broader objectives. Among these, it recommends following developments for:
Direct access to
Notes
- ↑ Pomey et al. (2000) in A system of Health Accounts 2011, revised edition page 100.
- ↑ A System of Health Accounts 2011, revised edition page 100.
- ↑ A System of Health Accounts 2011, revised edition page 100.
- ↑ A System of Health Accounts 2011, revised edition page 100.
- ↑ Preventive actions such as check-ups provided during a contact with a general practitioner might be included in expenditure for curative care.
- ↑ A System of Health Accounts 2011, revised edition page 164.
- ↑ A System of Health Accounts 2011, revised edition page 122.
- ↑ A System of Health Accounts 2011, revised edition page 145.
- ↑ A System of Health Accounts 2011, revised edition page 135.
- ↑ A System of Health Accounts 2011, revised edition page 38.
- ↑ Strategic Plan 2020–2024 DG Health and Food Safety (DG SANTE).
Online publication
Methodology
General health statistics articles
- Health (hlth), see:
- Health care (hlth_care)
- Health care expenditure (SHA 2011) (hlth_sha11)
- A System of Health Accounts 2011, revised edition
- Healthcare expenditure (SHA 2011) (ESMS metadata file – hlth_sha11_esms)
- European Commission – Directorate-General for Health and Food Safety – European core health indicators (ECHI)
- European Commission – Directorate-General for Health and Food Safety – Health systems performance assessment
- European economy – The 2021 Ageing Report: Economic and Budgetary Projections for the EU Member States (2019–2070)
- European economy – The 2021 Ageing Report: Underlying Assumptions and Projection Methodologies
- OECD – Country health profiles
- OECD – Health publications
- World Health Organization (WHO) – The global health observatory (GHO)
- World Health Organization (WHO) – Health system governance